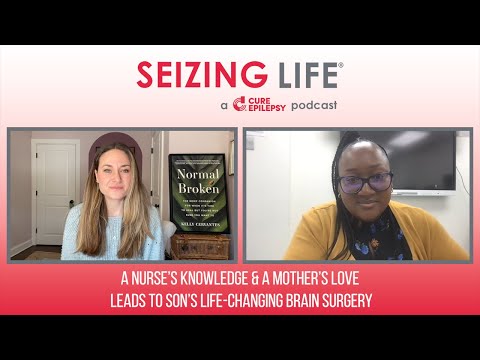
A young son’s journey from the onset of focal seizures to a devastating diagnosis of Rasmussen’s Encephalitis to a life-changing brain surgery.
Episode Overview
This month on Seizing Life® a nurse and mother shares her young son’s journey from the onset of focal seizures to a devastating diagnosis of Rasmussen’s Encephalitis to a life-changing brain surgery.
Episode Transcript
Kelly Cervantes: Hi, I’m Kelly Cervantes and this is Seizing Life, a monthly podcast produced by CURE Epilepsy.
Today on Seizing Life, I’m happy to welcome Jamilah Doyle to the podcast. Jamilah’s son, RJ first developed focal seizures at the age of four. He was diagnosed with a rare neurological condition called Rasmussen’s encephalitis when he was six years old.
Faced with very few good treatment options, Jamilah, who is a nurse practitioner, chose surgery for her son. She is here to share RJ’s epilepsy journey and offer her insights on advocating for your child’s epilepsy care. Jamilah, thank you so much for joining us today. To kick things off, can you talk to us a little bit about RJ and also when he had his first seizure?
Jamilah Doyle: RJ, he goes by Randall, but his nickname is RJ. I could brag about him all day. His first seizure occurred in April of 2019. He was at daycare with my parents and my father called to inform me that RJ had a seizure, and I immediately stopped what I was doing. I left work and I went straight to the daycare. The ambulance arrived right behind me.
We rolled to the nearest hospital, children’s hospital nearby, and we pretty much was in the emergency room, in the back area in a room, just me and him. He was still in that postictal state where he was kind of just screaming, kicking, not able to really kind of speak and take commands at the time. So all I could do was just wrap my arms and my legs around him. And I just wrapped my arms around him and I just rocked him to sleep and sang to him the best way I can to just relax him and calm him.
Kelly Cervantes: It’s amazing what a mother, caregiver’s love and touch can do for a child in that situation. What were you told while you were in the ER and what instructions were you given when you went home?
Jamilah Doyle: I was just told to follow up with his primary care doctor and that it’s not abnormal for kids to have a seizure maybe once or twice in their childhood.
Kelly Cervantes: And so you followed up with the pediatrician, but the follow-up appointment couldn’t happen soon enough?
Jamilah Doyle: Correct. And even after we did follow up, I still didn’t get a definitive answer as to what was going on and why it happened. Unfortunately, he was one of those cases that it had to get worse before it got better. But we actually experienced another seizure a week or two after, and that’s when I finally got to see the actual neurologist and we were starting on a medication called Keppra.
Kelly Cervantes: At this point, have they diagnosed him with epilepsy?
Jamilah Doyle: No. So according to the provider at the time, a child had to have so many seizures in a time in order to be diagnosed with epilepsy.
Kelly Cervantes: Two unprovoked seizures, which he’d had. So no epilepsy diagnosis, they start him on Keppra. Did it work?
Jamilah Doyle: No, it did not work at all. The next week, maybe two, we was back, another seizure. And Randall never had generalized seizures, which people hear seizure, that’s what they immediately draw to. Randall had focal seizures, so it’s almost like him staring off and he was able to follow commands, but he was just kind of nonverbal and he’ll just stare off. So imagine you having a conversation with your spouse and they’re in the middle of a good football game and they’ll ignore you for 30, 45 seconds and then come back to you.
Kelly Cervantes: So the medication isn’t working. You still don’t have an epilepsy diagnosis. I can’t imagine how frustrated and helpless you felt. What actions were you taking? What were you thinking at this time?
Jamilah Doyle: Well, things actually, they couldn’t move quick enough for me. We tried several medications. So after Keppra, we was put on another secondary medication, and that’s when we finally was told, “Yes, he officially has epilepsy.” We tried that medication and then we tried another medication. We tried the keto diet. We tried everything. Taking away foods with dye in them. It was a lot and nothing was really working for us at all.
Kelly Cervantes: Yeah, that period of time to me always felt like the doctors were just throwing darts at a board and hoping something stuck, but it wasn’t working. At what point did you decide that maybe it was time to get a second opinion?
Jamilah Doyle: By month three. By month three, I had a conversation with his doctor because we was on multiple seizure meds at one time. And I had a conversation with his doctor and I told his doctor, I said, “It doesn’t really seem like we’re getting anywhere, we’re finding out what’s going on because all the testing was coming back negative.”
I told him, I said, “So you have three more months to figure out what’s wrong with my son.” I told him, “I don’t know who you need to call. I don’t know if you need to go back in your books and find out what’s going on, what could this be, talk to a more seasoned neurologist, but we need to figure out what’s going on.”
Kelly Cervantes: And I’m curious, do you know, was that neurologist and epileptologist specifically or were they a general neurologist?
Jamilah Doyle: He was a general peds neurologist, that I know for sure.
Kelly Cervantes: Yeah, which gets us to the point of not every-. Or not every neurologist is an epileptologist, but every epileptologist is a neurologist. And I think that’s it’s such a frustrating thing as a parent and certainly as a patient when you’re advocating for yourself or for someone else to not know these differences and how vital they are for the care of ourselves or our loved ones. So eventually you did seek out that second opinion. What was that experience like?
Jamilah Doyle: So I actually went on a Epilepsy Foundation website and start trying to find a pediatric neurologist because it’s such a shortage of them in the US. So that’s where I found his pediatric neurologist, Dr. Ahmad and I called to schedule an appointment. Unfortunately, it was kind of extensive. It was three months out.
However, we booked the appointment and we was just on from there. Once we finally met in November, I was actually happy. November 2019 we met. I was proud because it was one of the days where he was just having his focal seizures, and so she got a chance to see them for herself. And the day we met, she saw them. She knew immediately what to do. She gave him Topamax, and that night he took it. The next morning, his seizures had stopped.
Kelly Cervantes: Wow.
Jamilah Doyle: Yeah. So after seven controlled substances of what he was on, that one medication stopped and her plan was to start weaning him off the Keppra, the Vimpat, the… it was the EPIDIOLEX, the CBD oil, DEPAKOTE. So she decided that they never worked to begin with, so it didn’t make any sense to continue to give them.
Kelly Cervantes: Yeah. It’s incredible what a difference finding the right doctor for your child can be and the hope that that can provide.
Brandon: Hi, this is Brandon from CURE Epilepsy. Do you have questions about seizures, medications, treatments, or other areas of epilepsy? CURE Epilepsy’s new video series, Epilepsy Explained, provides answers to help you better understand the basics of epilepsy. Each month, a different expert offers short, easily understandable answers to questions from our community about a particular area of epilepsy.
Doctors and researchers who are leaders in their field will cover questions about seizures, diagnosing epilepsy, medications, surgery, and many more topics. New episodes of Epilepsy Explained will be available on CURE Epilepsy’s website and YouTube channel on a third Wednesday of every month. Now, back to Seizing Life.
Kelly Cervantes: How long did RJ remain seizure-free?
Jamilah Doyle: He remained seizure-free from November of 2019 all the way until June of 2020. However, I will say that if we could backtrack before I met her, his behavior started to change around August of 2019. And so that was another reason why I was seeking a second opinion. He became to be very aggressive. He wasn’t patient. And my son, he’s very kind, very gentle. He loves to hug. And a lot of things would trigger him, and he would respond real negatively, and I couldn’t quite gather why he was responding that way.
He also began to experience numbness and tingling in his left leg, which at the time he was five maybe. So he was describing it as water or fire in his legs. That’s how he would describe it, and he would just fall. So by the time we saw her, she had enough history on him, gave us the Topamax, and we were seizure-free from November 2019 all the way until June of 2020.
Kelly Cervantes: And did the Topamax help with the numbing in his legs as well?
Jamilah Doyle: It did. It actually did. When we got to June of 2020, we was of course in COVID. So because of the changes that he was experiencing towards the end of 2019, I requested an MRI and CT to see the changes because I had never did one with that doctor. The last one was with the first, the initial provider. And so I fought with the insurance company because they said it was not medically necessary.
Then I decided to write the insurance company, talk to them, got it approved. And we were supposed to go in March of 2020, but that was right when COVID hit. So it was elective procedure, so it wasn’t medically necessary. It wasn’t urgent. So they just decided to postpone it. And then we got to June. He broke out into a cluster of seizures where he would have a focal seizure every, I would say two to three minutes, and they would last for 45 seconds. And I tried to keep him at home and manage things at home given my background. But once it got out of hand, I just couldn’t do it anymore. So we went to the emergency room.
Kelly Cervantes: So I want to pause for a moment in the story because you mentioned your background, and I want to dive into that a little bit because I think it is so important to understanding your expertise and your knowledge because what you’re talking about, fighting with the insurance company and knowing how to do that, understanding how to find a second opinion, and that you wanted him to have another MRI, these are all things that you know because you are a nurse.
You’re now, a nurse practitioner, and that is such valuable knowledge and experience to have as you’re walking into the epilepsy world because it is so complicated. And I’d love to hear from you how you feel like that helped you advocate for RJ?
Jamilah Doyle: It helped me tremendously. I tell people God made no mistakes as far as giving him to me because I was able to navigate it so well. Although my background is primarily in women and children’s health, I knew first and foremost having seizures was not normal. I knew that imaging was required and I just kept doing as much research as possible to just try to figure out how I could help him and just do the best thing that I can.
The most helpless feeling as a mother is just not being able to just take it away and to protect your child. So I just did the best I can with what I had asked, the right questions. I found support groups on Facebook of other neurologists and other patients who were going through the same thing. So they kind of helped me navigate it as well.
Kelly Cervantes: Yeah, building out that community and that network is just so incredibly important. And the research that you talk about, I mean, I can’t even… The number of hours that I was Googling until three o’clock in the morning is overwhelming to think about. I want to get back to the medical odyssey that you went on here, you fought for this MRI. COVID happens, everything gets pushed back. But you do finally get this MRI done. And just as it sounds like RJ is really taking a downward turn, what did the MRI show?
Jamilah Doyle: His MRI and CT show right frontal lobe brain atrophy, atrophy, meaning tissue death. And he was actually diagnosed with COVID while we were there. So he was diagnosed with COVID, and we was also given the diagnosis of Rasmussen’s encephalitis.
Kelly Cervantes: And what is that?
Jamilah Doyle: So the simplest way that I can explain it is it’s like a childhood form of Alzheimer’s. The brain itself begins to attack itself and it just dies off. And that’s exactly what was going on. I watched the MRI and CT on the screen as the provider. The doctors came in and showed it to me, and I immediately just collapsed. It was a lot.
Kelly Cervantes: Yeah. Yeah, a whole freaking lot. Rasmussen’s encephalitis, is it a virus? Is it a genetic condition? How does it appear in the body?
Jamilah Doyle: So it’s an autoimmune disorder and it’s 600 cases in the US so it’s not a lot to really know about it. I’ve heard things about the extra T-cells that come to attack the brain, but it’s not a lot of information on it. Like I said, it is one of those things that has to get worse because most kids, seizures, you would think the seizure is causing the brain death, but it was really the Rasmussen. So the seizure was just a symptom.
Kelly Cervantes: Yeah. So you receive this terrifying diagnosis, and what are you told in terms of treatment and prognosis?
Jamilah Doyle: Actually, due to my emotions, I was actually left alone for a minute. After they left, the first thing I said to myself was, “God, you can have it.” Because I felt like I’ve done the best that I can do as a mom, as a person to give him the best care that he needs and find the right doctors. And I had been a nurse for, I’ve been a nurse since 2011, so here we are years later. I had never heard of this, did not know how to navigate it.
It was just a lot of unknowns. And I immediately, they gave me a moment. I immediately called my sister first, my dad, and then I called my husband and told them what was going on. And of course, everybody came and we met outside. But while everybody was in route, I was Googling. I was Googling treatments, I was Googling prognosis, I was Googling to see what his life would eventually look like as an adult, just to prepare myself and him for what was to come.
Kelly Cervantes: And so what is the prognosis and what have the treatments been?
Jamilah Doyle: So he goes on to live a normal life with some deficits, of course. I have read that a lot of individuals do go on to have Alzheimer’s later on in life, dementia and osteoporosis. But ultimately the treatment plans that were provided, it was of course one, was do nothing, which was never an option.
The second one was to do steroids, which I read about it and it left some changes. It kind of slowed down the process, but it doesn’t stop it. And the best one of all was the hemispherectomy, and that’s the decision I went with. I instantly made up my mind that that’s what we was going to go with.
Kelly Cervantes: Not an easy decision to make, just brain surgery, splitting the two halves of the brain.
Jamilah Doyle: There you go.
Kelly Cervantes: No big deal. Right? So I wonder if you can walk me through your process in finding a neurosurgeon to operate on RJ?
Jamilah Doyle: That was actually kind of fun. I actually interviewed the provider who wanted to do his surgery. So where he was originally receiving his care and the neurologist that diagnosed him, of course, by the diagnosis being so rare, the neurosurgeon at that particular hospital wanted to do his surgery. And it was a hospital that I’m also employed at, and I was willing, but I wanted to have a conversation first, just get to know him.
I saw all the certificates, but I wanted to know the person. I wanted to know their background as far as how often they do these surgeries. So we did set up a meeting where I was able to talk to him and amazing doctor. So I asked him, I said, “How often have you done this surgery?” And he was like, “Oh, I do it all the time.” And I said, “How often do you do it on kids?” And that’s when he got quiet and he was like, “Not so often, but I have done it before.” And I told him, “I appreciate you meeting, but I need somebody who deals with kids’ brains. They’re different.”
Kelly Cervantes: Why was that important to you?
Jamilah Doyle: Well, like I said, they’re really different. And with him being six at that time of his diagnosis, I knew just based off once again, my background that the neural pathways, how the brain kind of reconstruct itself, that kind of cuts off at age seven. So I knew we didn’t have long to think about it. And I wanted him to have the best optimal outcome.
Also, I asked him about his technique. Long time ago when these were first done, they left a huge question mark scar on the side of a lot of kids’ heads, which I know can leave some body image, somebody dysmorphia. And I did not want that to have to be a concern for my son. So once again, I hoped right back on Google and I started looking up Rasmussen’s, and then I started looking up neurosurgeons.
And actually one of the articles that I read about Rasmussen’s, the neurosurgeon had actually just transferred to a hospital here in Chicago from a children’s hospital in Texas. And so I called her up, of course, they was like, “Well, her schedule is really backed up.” And I’m like, “Just tell her my son’s case, just tell her.”
And they called me back within a couple of days and was like, “We want to meet you.” And we started from there. And she didn’t have to convince me much. I was well aware of her background. I was well aware of the articles that she had written. I was well aware of her technique, that is laparoscopic, meaning it’s with a robot. So it decreases the chances of bleeding. It increased healing time where it’s quicker and it’s not so invasive.
Kelly Cervantes: That certainly helps make that decision just to touch a bit easier, when you’re working with someone who is that experienced. And how fortuitous that she had just moved to Chicago where you lived. So RJ was six at the time of the surgery. I mean, aware enough to know that something is wrong and to have to be prepped verbally about what is happening. How did you explain it to him what was about to happen?
Jamilah Doyle: He understood that he was having seizures. He was actually able to let you know, “I just had one.” So he was able to identify them. Get him ready for surgery was, it was tough, but we did it. He knew my job, and I kind of went to him and I’m like, “Hey, buddy.” I’m like, “You’re going to go for a really intensive brain surgery.” I said, “But guess what?” I said, “Mommy has some really cool friends who’s going to help me take care of you, and we’re going to stop these seizures.”
And I told him, I walked him through the process of how the IV was going to start, which he had already had IV before. So we kind of played the game of, you’re super superhuman and in order for you to be like this amazing person, you need superpowers. So I would tell him like, “Ooh, you getting your superpowers, you’re going to be strong.”
So that was already planted inside of his head as we went through all the frequent hospitalizations. But he kind of took it pretty well. I told him, I said, “It was going to be tough.” I said, “But you can do it.” I said, “You can do anything.” And I told him, “You have all your family here.” I wanted him to know and understand that he’s loved and that he’s supported and that he got this. Like, “We got you. You’re going to do this.” He was a trooper.
Kelly Cervantes: I love it. What did the recovery look like from the surgery?
Jamilah Doyle: His surgery, first off was 13 hours long.
Kelly Cervantes: Oof.
Jamilah Doyle: The longest surgery.
Kelly Cervantes: [inaudible 00:24:06]
Jamilah Doyle: We were the first family in, the last family out, but we met a lot of great families during the process. We played Uno. Before playing Uno, I took my final exam. It was my finals, so I had to take my final exam.
Kelly Cervantes: Oh my gosh.
Jamilah Doyle: Yeah, I took my final exam. They provided me with a space to take my final exam. I did that. We played Uno, Jenga, spades, anything to pass the time by. They kept us updated frequently. At the end of surgery, I just immediately grabbed his hand, almost like when that baby is firstborn and you put your pinky there, I put my hand there.
And I still have the picture. And I told him like, “We got this.” And he said, “Mama?” And I was like, “Yes, baby, it’s mommy.” And we stayed at the hospital from start to finish with the hospital and the rehabilitation center. He was in and out in 30 days.
Kelly Cervantes: Okay. And what kind of rehab did he require?
Jamilah Doyle: So he required two to three weeks of rehab, inpatient. We were discharged to outpatient rehab, and that was three days a week for three hours.
Kelly Cervantes: And what were you rehabbing? What was he having to learn how to do again?
Jamilah Doyle: Well, initially, of course, rehab always starts in the hospital. So by day two, he was walking again.
Kelly Cervantes: Oh, wow.
Jamilah Doyle: He did have to learn how to swallow because he did fail two swallow evals, so we did have to teach him how to chew his food, how to get his neck support back. And when we left, he was walking with a little forearm crutch. So he had to learn how to pay attention again, how to refocus himself. Math.
Because he was such a great reader, so he had to learn how to read and articulate his words better. He went through a lot. Unfortunately, during his time, he did forget how to ride a bike, and he later on just recently regained that back. So it’s still a uphill battle, but he’s doing great.
Kelly Cervantes: That’s amazing. Post surgery, what are the benefits that you have seen? You’ve talked about how difficult the rehab was, but how worth it was and how he’s walking and riding a bike. What are some of the other differences that you’ve noticed? It’s been three years now since the surgery, is that correct?
Jamilah Doyle: Yep. A little bit over 1600 days. I keep count. Yeah. And we have a hemi-versary. So every year on his anniversary, we call it a hemi-versary. So we go out, he’ll bake cakes, whatever he wants to do. We’ll celebrate with his friends because his classmates supported him heavily through the process.
Kelly Cervantes: So he is seizure-free as of this time?
Jamilah Doyle: Yes. He’s seizure-free. He’s been seizure free since then. He’s been taking off most of his medications. We’re only on one. He does Taekwondo, so he’s a yellow belt working towards his orange belt. He plays basketball for Special Olympics. He runs track. He’s actually heading down state in two weeks because he did place first in his school for his grade level for basketball.
So we’ll be going downstate to Normal Illinois and supporting him down there. He’s a pretty amazing kid. He rides his bike now. I tell people I had three kids in one. I had the one that I delivered, then I had the one that I had during the seizures, and I have the one after.
Kelly Cervantes: That’s incredible. He sounds like a truly, truly amazing person. And what does his prognosis look like? He’ll go on to lead a typical life?
Jamilah Doyle: Yeah. He’ll go on to live a typical life. Of course, it’s some deficits, like he is still struggling with reading and math because their frontal lobe kind of helps with just logical thinking and processing. And impulsivity, so we do have a diagnosis now of ADHD. But none of that matters that I have him. He’s healthy. He’s fun. He has lots of friends, family. He know he’s loved and cared for. He loves to cook, so I tend to foster things that can help him develop some type of career. He’s getting there. He’s doing amazing.
Kelly Cervantes: That’s so incredible to hear. I love that. And I love that he’s cooking. That’s so much fun. One day taking over for you in the kitchen, I’m sure.
Jamilah Doyle: I hope so. I just want him to just be great. I want him to just know how to pay your bills. Just be a good person. Be kind. That’s my dream for him.
Kelly Cervantes: Absolutely. Now, we’ve spoken about advocacy and racial biases before on this podcast, and I feel like I would be remiss not to ask you. I know that you felt like you had a leg up because of your medical background. However, I wonder if you felt like you had any differences or additional challenges because of the color of your skin?
Jamilah Doyle: I would definitely say yes, I did. I’ve never been one to boast who I am when I go in, I like to kind of watch and observe because I want to see what your integrity lies. I tell people integrity is important, and that means doing the right thing all the time, even when nobody is looking. And a lot of times I was talked at and I would have to ask questions. They would want to do things that did not quite make sense.
And I would have to ask, “Are you asking me or are you telling me?” And then I would ask, “I need for you to support this.” And as I asked more questions, then everybody say, “Are you medical?” And then I say, “Yes.” And then that’s when everybody tones change. When I had to assert myself with the first provider, and I knew that you are supposed to see us within 24 hours of admission, and we were over 24 hours of being admitted, and I’m not just speaking in the ER.
I’m speaking of a bed upstairs. You are supposed to see me within 24 hours and you have not. I had to have a sit down with him, “Say what you mean and mean what you say. If you want to be a man of integrity and continue this relationship with me and my son, I need for you to show up. I need for you to be present. I need for you to be available.” Definitely, it definitely played a big role in it. And I can’t imagine if I didn’t have the background to advocate for him and to get things done, what things would be.
Kelly Cervantes: Yeah. Jamilah, is there advice that you would want to share with other parents who are either navigating a new diagnosis or even are years into it, but still struggling to find the answers? Still struggling with perspective and the grief from the realization that maybe life isn’t going to look quite like what they thought it would. What advice do you have for those parents and caregivers?
Jamilah Doyle: I would definitely say advocate. Advocate, advocate, advocate. Ask questions. Research things. Talk to people. Lean on your community. Too often we tend to kind of want to suffer alone, and the world was not meant to be that way. People were put on earth to support each other, and if we just have a little bit more of that, the world would be a whole lot better place. And they say it takes a village. It takes a village. And adults need villages too.
Kelly Cervantes: 100%. That’s pretty incredible advice. Jamilah, thank you so much for sharing your journey, for sharing RJs story with us today, and I just wish you and your family all the best moving forward.
Jamilah Doyle: Thank you so much. It was a pleasure being here.
Kelly Cervantes: Thank you, Jamilah for sharing your son’s epilepsy journey and offering advice on navigating epilepsy care as a nurse and mother. The mothers who started CURE Epilepsy over 25 years ago came together to improve care options for their children and push research toward finding a cure. To date, we have raised over $90 million to fund epilepsy research and other initiatives.
We have seen great advances in treatment options, epilepsy, genetics, and our understanding of the complexities of epilepsy. But we continue to push science toward our ultimate goal, a cure. If you would like to help us achieve our goal of a world without epilepsy, please visit www.cureepilepsy.org/donate. Thank you.
Legal Disclaimer: The opinions expressed in this podcast do not necessarily reflect the views of CURE Epilepsy. The information contained herein is provided for general information only and does not offer medical advice or recommendations. Individuals should not rely on this information as a substitute for consultations with qualified healthcare professionals who are familiar with individual medical conditions and needs. CURE Epilepsy strongly recommends that care and treatment decisions related to epilepsy and any other medical conditions be made in consultation with a patient’s physician or other qualified healthcare professionals who are familiar with the individual’s specific health situation.