Access to medications to treat and control Seizures
Access to medications prescribed by your physician is important to both control seizures and ensure the best possible outcome for your health. However, it can be difficult to understand and navigate how prescription drugs get from the manufacturer to the pharmacy and what determines whether or not your insurance will cover the cost. The health insurance and prescription benefit ecosystem in the United States is incredibly complex. The information below provides a high-level description of the process so that you can better understand the various players and know where you may encounter obstacles to obtaining your medicine.
Epilepsy Medication Manufacturers
Manufacturers are the companies that produce pharmaceutical products. You may be familiar with some of the companies that manufacture antiseizure medications. For example, SK Life Science manufactures Xcopri® (cenobamate). UCB manufactures Brivact® (brivaracetam), Vimpat® (lacosamide), Fintepla® (fenfluramine), and Nayzilam® (midazolam nasal spray). Jazz Pharmaceuticals manufactures Epidiolex® (cannabidiol).
Branded, Generic and Branded Generic Medications
The prescription medications that manufacturers produce are either branded, generic, or branded generics. Brand-name medications are drugs that have been approved by the FDA and have patent protection so that no one else is permitted to manufacture them. For example, UCB was the original manufacturer of the drug levetiracetam, known by its brand name Keppra®, when it was approved by the FDA in 1999.
The duration of the patent protection for each drug varies, but once it expires, other companies are then allowed to apply to manufacture the drug in addition to the original branded manufacturer. Keppra® lost its patent protection in 2008. At that point, several other manufacturers obtained approval from the FDA to manufacture a generic version of leviteracetam.
A generic drug uses the same chemical name that the branded drug uses (e.g. leviteracetam) and it contains the same active ingredient as the branded medication. It has the same quality, the same safety, and the same strength as the branded drug. However, the generic may differ in several ways. It may contain different inactive ingredients, and importantly, the FDA only requires that the generic drug be “bioequivalent” to the branded drug. Bioequivalence is declared when there is no significant difference between the generic drug and the reference drug in the rate and extent to which the active ingredient becomes available when administered at the same dose under similar conditions and in an appropriately designed study. This allows for some small variability between a branded and generic drug.
So, if you fill a prescription for levetiracetam or any other medication at the pharmacy, there is a high likelihood that you will receive a generic version. And usually, there are several manufacturers of each generic medication. Therefore, it is possible that when you are filling a prescription for levetiracetam or lamotrigine or carbamazepine, you may receive a drug manufactured by a different pharmaceutical company from month-to-month or from pharmacy-to-pharmacy.
One last category of prescription medication is a hybrid called a branded generic. These are generic drugs that the FDA has approved, but the manufacturer has decided to give them a brand name instead of simply utilizing the chemical name. An example of this is the antiseizure medication Vigadrone® which is a generic form of vigabatrin, but branded with its own name. Branded generics are often marketed like branded medications and may have similar patient support programs that you see with branded medications such as a call center, copay cards, and patient assistance programs. Branded generics often cost more than generics, but less than their branded counterparts.
Your pharmacist can tell you if you are receiving a generic version of a drug or you can look at the prescription information to find out.
Wholesale Distributors
The primary way that drug manufacturers get their medications to pharmacies, and ultimately patients, is through drug wholesalers such as McKesson and Cardinal Health. Wholesalers buy large quantities of the drug from the manufacturer, manage the inventory, and then distribute it to retail chain pharmacies (e.g. CVS), independent pharmacies, specialty pharmacies, mail-order pharmacies (e.g. Express Scripts), hospitals, long-term care and other facilities.
Generally, the public has no interaction with wholesalers. These are business-to-business transactions.
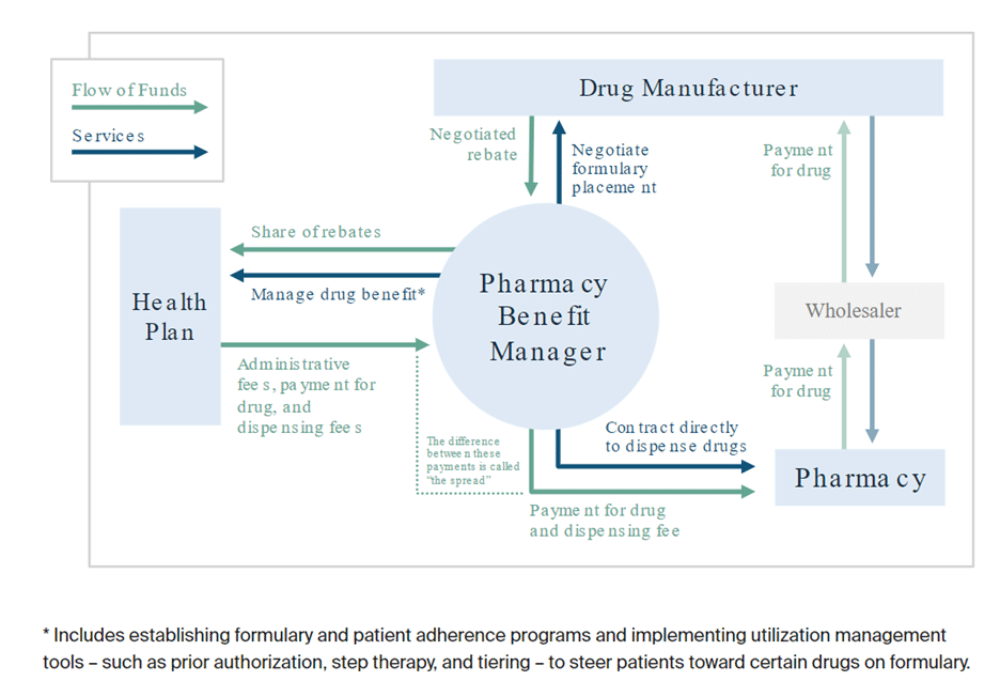
Pharmacy Benefit Managers
Pharmacy benefit managers (PBMs) are companies such as Prime Therapeutics, Express Scripts, or CVS Caremark, that contract with health insurance companies (e.g. Blue Cross Blue Shield, United Healthcare, etc.) to manage the prescription benefits for people enrolled in their health plans.
The PBMs contract directly with the pharmacy chains (e.g. CVS, Kroger, etc.) to set agreed upon pricing for the cost and reimbursement of prescription drugs. The PBMs also work with the health insurance companies to establish and/or maintain a drug formulary. The drug formulary (sometimes called a Preferred Drug List) is a list of branded and generic drugs that the health insurer will cover in a specific health plan. Lastly, the PBMs process and pay drug claims from the pharmacy.
So, if you go to your corner pharmacy to pick up a prescription, the pharmacy technician will process the prescription by using the computer to “ping” your health insurance plan and see what drugs are approved on the formulary, and what the cost or co-pay will be to you. If you are prescribed a brand name drug and a generic version is available, this may be where a switch is made because of the formulary associated with your health insurance plan.
Pharmacies
Pharmacies are the licensed bodies that are able to dispense prescription medications to the public. You are familiar with the pharmacy in your local CVS, Walmart or Kroger store. However, there are other types of pharmacies besides these retail chain pharmacies. There are also specialty pharmacies, mail-order pharmacies, and on-line pharmacies that may supply your antiseizure medications.
The price of prescription drugs is not regulated and can vary dramatically from pharmacy to pharmacy. Even if you have health insurance, it is important to compare prices if there is an out-of-pocket cost or co-pay with your medication. Figuring out where to go for the lowest prices on your medications can add up to significant savings.
Retail Pharmacies
Pharmacy chains such as CVS, Walmart, Kroger, or networks of independent pharmacies such as Good Neighbor Pharmacy buy the medications from the wholesaler (or sometimes directly from the manufacturer) and make them available in their retail stores so that it is easy for patients to fill their prescriptions. They are the last stop in the supply chain for the consumer. The retail pharmacies generate the prescription drug claims that are then sent to the pharmacy benefit managers and health plans (insurers) to determine if the prescription drug will be covered and, if so, how much it will cost the patient.
Speciality Pharmacies
Specialty pharmacies are a type of pharmacy that is licensed by the state and is used primarily when the cost and/or the complexity of the therapy require increased management. The use of specialty pharmacies has increased dramatically in the past ten to fifteen years. Drug manufacturers decide which specialty pharmacy or pharmacies they want to distribute their medication through.
Drug manufacturers may choose to use a specialty pharmacy instead of going the traditional route of retail pharmacies for a variety of reasons. For example, the medication may require special storage and handling such as refrigeration. The medication may need to be administered by injection or infusion. The medication may have a Risk Evaluation and Mitigation Strategy associated with it, so it has special requirements before it can be dispensed, such as an eye exam or an echocardiogram. The medication may have an extremely high cost or be for an extremely complex, rare or chronic condition.
Several antiseizure medications can only be obtained through specialty pharmacies, including Sabril® (vigabatrin), Achtar® Gel (corticotropin injection), Epidiolex® (cannabidiol), and Fintepla® (fenfluramine). If you are prescribed a medication that is only available through a specialty pharmacy, your prescribing physician’s office will let you know. You will likely have to fill out a special intake form to get the prescription. You will not get a paper prescription nor will an electronic prescription be sent to your corner pharmacy.
Medications that are dispensed through a specialty pharmacy usually come with a significant amount of support services. You will likely have access to a call center to help ensure that your prescription gets filled. There is a good chance that there will be financial support services such as a co-pay program to help you cover the cost of the medication. You may even have access to a nurse or other healthcare professional to answer your questions.
Mail-order Pharmacies
A mail order pharmacy is another type of pharmacy that contracts with your health insurer or pharmacy benefits manager. If your health plan has a mail order pharmacy, you may choose to have your medication delivered directly to your mailbox instead of having to go to the corner pharmacy and pick it up. Examples of mail order pharmacies include Express Scripts, OptumRx, CVS Caremark, and Walmart Pharmacy Mail Services.
Your copay and coverage may differ at a mail order pharmacy than at your local retail pharmacy. Oftentimes, filling your prescription at the mail order pharmacy is cheaper than getting it from your local pharmacy, and they often fill a prescription for 90 days instead of just 30 days, which may also save you money. However, it may take longer to receive your prescription from a mail order pharmacy and mail can be unpredictable. This is important to consider if you have a life-threatening condition that requires medication or if you need your prescription immediately.
Cost Plus Drugs, Amazon and other newcomers
In recent years, some new options have come to the marketplace offering alternative models for getting your prescription medications. These can be very good options for people who do not have prescription drug insurance, and even if you do have prescription insurance, it may be worth comparing your out-of-pocket cost for the medication with their pricing.
Cost Plus Drugs
Cost Plus Drugs was founded by serial entrepreneur Mark Cuban in 2022. The business model is founded on providing low-cost medicines with transparent pricing. The cost for each medication that Cost Plus Drugs stocks is its purchasing price plus a 15% mark-up, $3 for labor, and $5 for shipping. You can see the pricing for each of the drugs that it stocks on its website. Cost Plus Drugs is able to offer low pricing because it eliminates the middlemen in the supply chain that we described above (wholesalers and PBMs).
Cost Plus Drugs is not a full-service pharmacy; it only supplies selected generic drugs. However, it does have a very robust list of hundreds of generic medications including many antiseizure medications.
Amazon
Amazon launched Amazon Pharmacy in 2020 as a digital drugstore. It is a full-service pharmacy and offers both generic and branded medications. You can use your health insurance pharmacy benefit or you can pay out-of-pocket for medications. Amazon Pharmacy offers transparent pricing, so that you can put in your information and see what the cost for your medication(s) will be. Your medications are mailed to you, including free 2-day delivery for Amazon Prime members.
Amazon Prime members get other special perks including a small set of generic medications for $5 per month, including several antiseizure medications. There is also a new feature where manufacturers’ discount coupons for branded medications are automatically applied to the cost of a prescription when available. This ensures that a patient getting a branded prescription filled is paying the lowest out-of-pocket cost available. This feature is only available for products from some manufacturers right now, but Amazon Pharmacy is working to add more coupon selections over time.
GoodRx
GoodRx is a company that gathers current prices and discounts to help you find the lowest cost pharmacy for your prescriptions. It offers a competitive price by looking across the various retailers, including Walmart, Costco, and CVS. That price is often cheaper for the consumer than the cash price you would be offered at the register, which is typically highly inflated.
GoodRx also offers free discount cards and coupons for consumers to take to the pharmacy, often allowing them to get a lower price. In addition, it offers membership programs that may save you more money for a small monthly fee. GoodRx markets its service to the ~30 million Americans who are uninsured, as well as to people with high deductible plans who might still get a deal on their generic medications.
Others
There are also several competitors to GoodRx (e.g. pharmacychecker.com, singlecare.com) and many online pharmacies as well. It is definitely worth the effort to price shop if you do not have prescription insurance or if you have a high co-pay or co-insurance out of pocket cost for your medication.
Health Insurance and Prescription Drug Benefits
PRIVATE HEALTH INSURANCE
Private health insurance, also known as commercial insurance, is provided by employers or can be purchased by individuals directly from insurance companies. Most health insurance plans provide some sort of prescription drug coverage or prescription drug benefits. The exact type of coverage varies from plan to plan and the type of medication that you need. A small percentage of prescription medications are covered by your medical benefit instead of your pharmacy benefit, but that is more the exception than the rule.
Not all health plans cover all prescription drugs. If you need a drug that’s not covered, it can cost you hundreds to thousands of dollars out-of-pocket. Because of this, it is important to check your plan to see if the medications that you need are covered. This list of covered drugs is called a formulary. Check the plan’s formulary if you are looking to switch insurance plans due to a job change, a major life event (e.g. marriage), or even if you are considering changing plans within your employer’s options.
AFFORDABLE CARE ACT
The Affordable Care Act (ACA) was enacted to make affordable private health insurance available to more people, especially those who are uninsured. The law provides consumers with subsidies (“premium tax credits”) that lower costs for households with incomes between 100% and 400% of the federal poverty level (FPL). The ACA requires health plans offered on their marketplace to include prescription drug benefits. Information can be found at www.healthcare.gov.
PUBLIC HEALTH INSURANCE
There are several types of public health insurance including Medicaid, Medicare, and TRICARE.
Medicare is a federal health insurance program for adults aged 65 and over, younger people with disabilities, and those with permanent kidney failure or ALS (Lou Gehrig’s disease). It has different parts and options, such as coverage for prescription drugs.
Medicaid is a joint federal-state program that provides free or low-cost health insurance to low-income families and children, pregnant women, older adults, and people with disabilities. Although pharmaceutical drug coverage is an option benefit under federal Medicaid law, all states currently provide coverage for outpatient prescription drugs.
TRICARE is the uniformed services health care program for active duty service members (ADSMs), active duty family members (ADFMs), National Guard and Reserve members and their family members, retirees, and retiree family members, survivors, and certain former spouses worldwide. TRICARE includes a prescription benefit program.
Patients using Medicaid, Medicare, or TRICARE are ineligible to utilize many of the support programs provided by drug manufacturers including copay cards, starter packs, or free trials.
PATIENT ASSISTANCE PROGRAMS
Most manufacturers of branded antiseizure medications, and some generic manufacturers, have a Patient Assistance Program (PAP) to assist people in getting medications if they do not have health insurance and if they are not covered by Medicare, Medicaid, or TRICARE. Most of these programs will provide free medicine if you can demonstrate financial need. Each company has different requirements, but usually, you have to demonstrate that your income is less than some multiplier of the Federal Poverty Level (FPL). You can find information on the PAPs on each manufacturer’s website.
INDEPENDENT CHARITABLE FOUNDATIONS
Patient assistance programs run by independent charities help patients pay for the cost of prescription drugs. They generally are set up to provide assistance within specific disease states, regardless of treatment. Below are the links to a few of these foundations; however, this is not an exhaustive list:
- Pan Foundation (https://www.panfoundation.org/)
- The Assistance Fund (TAF) (https://tafcares.org/)
- RareCare (https://rarediseases.org/patient-assistance-programs/financial-assistance/)
BARRIERS TO ACCESSING MEDICATIONS
PRIOR AUTHORIZATION
Prior authorization (also called “preauthorization” and “precertification”) is a requirement by health insurers and/or prescription benefit managers that requires approval by the plan before they will provide coverage. This authorization is generally performed either by your doctor’s office, or the manufacturer of the medicine may have a customer service center that will take care of this approval for you. Following the process is no guarantee that the request will be approved; the benefits manager may deny the request.
Prescription benefits managers put prior authorizations in place so that they can evaluate whether they deem that the medication is necessary and is being prescribed appropriately. It is a cost-saving measure.
STEP EDITS
Step edits are a mechanism designed by health insurers and pharmacy benefits managers to control costs. Usually, but not always, this means that patients are expected to try cheaper drugs before trying more expensive drugs. Step therapy means trying less expensive options before “stepping up” to drugs that cost more.