Epilepsy Surgery
In the United States alone, approximately 4,000 surgeries are performed each year to treat epilepsy. In comparison, an estimated 100,000-200,000 patients may benefit from epilepsy surgery 1. This significant gap between the number of surgeries performed and the number for whom it could reduce or eliminate seizures could be filled by procedures that can more easily identify patients who are good candidates for surgery.
How Magnetoencephalography (MEG) can pinpoint the source of seizures
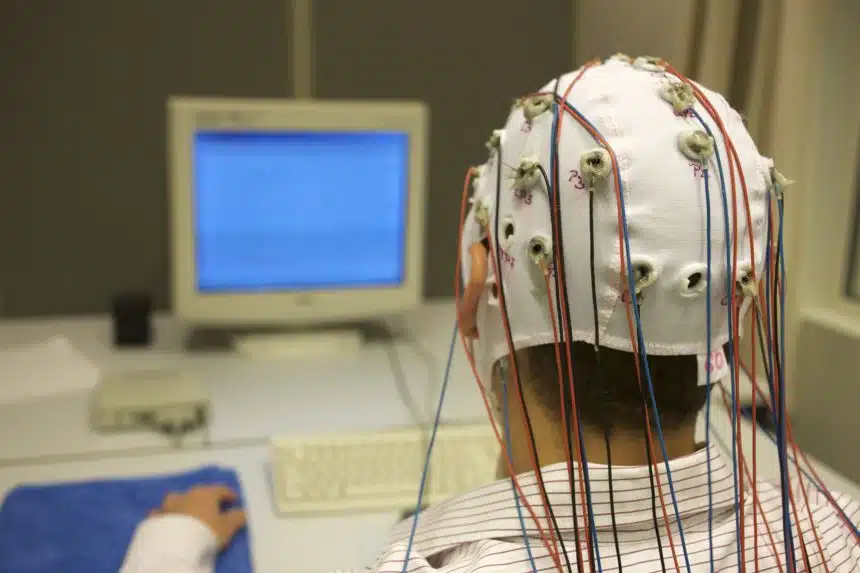
Magnetoencephalography (MEG) is the newest, most advanced technology that can help close this gap. MEG can pinpoint the source of abnormal brain activity and seizures 2, is painless, safe, and requires only 1.5-2 hours to perform. Ultimately, MEG can help surgeons decide whether a patient should pursue surgery. Use of MEG may allow more patients to be identified for surgery, and potentially lead to greatly reduced or no seizures.
How Magnetoencephalography (MEG) is a key part of the epilepsy surgery
In this webinar, viewers will learn how MEG is a key part of the epilepsy surgery evaluation, including information about the basics and safety of a MEG study, and hear about how MEG can help the surgeon by mapping key functions (speech, motor, and vision) onto their MRI for use in the operating room.
The webinar is intended for people living with epilepsy, their family members and caregivers, and anyone seeking to learn more about mental health and epilepsy.
1 Institute of Medicine (IOM) Epilepsy across the spectrum: Promoting health and understanding. The National Academic Press; Washington, D.C: 2012.
2 Gill MM et al. The use of PET/CT in pregnancy: A case report of malignant parathyroid carcinoma and a review of the literature. Obstet Med. 2018 Mar;11(1):45-49. doi: 10.1177/1753495X17724950. Epub 2017 Oct 9. PMID: 29636815; PMCID: PMC5888841.
Q&A Transcript
Can a MEG scan identify a misconnection with a hemispherectomy?
If someone’s had a hemispherectomy, just to make sure everybody understands that, it’s a big surgery, but basically what you’ve done is you’ve disconnected, if you will, one half of the brain and parts of that brain from the other half. You may have abnormal tissue that’s still in place. It can still generate a seizure. But the way I describe it to patients, it’s kind of like it’s on an island. It can’t spread from there to the rest of the brain or to the body, so it’s not really causing a seizure, even though it may have nothing but abnormal activity. It’s been disconnected, if you will, from the rest of the brain.
Usually, the best strategy for saying are we confident that’s disconnected is to do what we call a tractography. It’s a type of MRI imaging where they actually look at the pathways from those disconnected areas and they can see have they all been cut. And that’s probably the best way to look at those, because MEG picks up abnormal electrical activity, and that abnormal electrical activity is still going to be sitting there because it hasn’t left that area. The question is, is it confined there, and that’s where the tractography helps us better.
This individual writes about having a pacemaker and also having a MEG test. One of the concerns is that the device may cause too much noise for the MEG and how well can the MEG reading be cleaned up if a device like that is present?
Yeah, that’s a great question and an area that I didn’t touch on that I probably should have for purpose of the time. But their question is great because they’ve picked up on what I was saying at the beginning that the MEG is detecting these magnetic signals and anything that’s metal generates a magnetic signal, which is why we all know if you take a magnet, you go around, you can pick up other things that are metal, right? Pacemaker nowadays, most modern pacemakers and other metal implants, if you think about dental fillings, more common than pacemakers even, as well could have an associated magnetic field with them.
The brain is small by comparison. They can overshadow, if you will, the brain. In the past, those were a huge problem. With modern software, we usually, I almost say 100%, but we usually can filter the noise out from those and still get the data that we want in patients that have those. Whereas in the past, we kind of said, “Gosh, that’s a deal breaker, unfortunately.” Nowadays, we say, “You know what? Let’s look at it. Let’s get you in the room. Let’s see what we’re recording.” Even if it’s somebody that we can just kind of… I guess you would say get in the room and try it.
We’re not doing the full recording, but just say, “Let’s make sure we’re not overwhelmed by the noise,” we can just test them, if you will, to see because it’s easy to do. You just go in the room and lie down. It’s pretty simple to do. But most of the time, nowadays with our current machines and the software improvements, we’re able to record.
Is having MEG done something that insurance will cover if a patient is not wanting surgery, but wants to identify where the seizures are coming from?
Obviously, today’s focus was on patients with surgery, but many patients get MEG that are not surgery candidates where it’s still helpful. For example, for some patients that we say, “Gosh, we think we know your seizure type, but you’re responding a little bit differently than the normal person with this.” Sometimes using the MEG with EEG really helps refine, are we on the right track for what we think is the type of seizures that they have? It’s been used there.
It’s been used some in folks that have seizures, probably mainly in childhood where the seizures also may be associated with kind of developmental or language changes that are negative to say, “Okay, let’s see if we can tease out the relationship of these two to each other.” Obviously, today’s focus was surgery, but has it been used in other aspects of epilepsy aside from surgery? Yes, as well. The question they asked about insurance, at least at our center and I think most centers, obviously like any test we do pre-approvals so somebody’s not out of pocket, a surprise. None of us like that.
I get it. I don’t like that either. Usually, that’s not a barrier. I know when we see patients, even if they’re from other centers, I mean, I didn’t mention this either, but the nice thing is the MEG data can all be kind of put on disk, if you will, or printed out in picture form. It can go back to referring neurologists, neurosurgeon, whoever, for them to pull up. We can even put it on disk so they can pull it up on their own inter-operative equipment to register in their own OR as well. It’s portable from that standpoint.
If seizures are coming from scar tissue left from a Gamma Knife surgery in middle age following an AVM removal at 15, so long time ago, could MEG be useful?
Yeah, I think MEG could be, because a couple things with that kind of surgery is, one, if it was near critically functional areas, so language, motor, vision, it could help figure out that relationship. Even if it was not in one of those areas, if around where the prior abnormality is on MRI, if all of those make dipoles line up all around that, it’s really telling you, it’s like a big arrow saying, “This is the problem. This is why you’re still having seizures.” And then obviously that’s a discussion with what are my options to get rid of that problem.
I’m amazed at the resolution that MEG has. This person is asking about the precision. I mean, clearly, it’s very precise, but is it ever inconclusive?
There are times. Just like any test, can you have an inconclusive test? Sure, you can. I would say the benefit of the MEG is that that happens. I will say I’ve not done this a lot, but we’ve done this some, we’ve had patients, their first has been inclusive. We really thought, gosh, we really need to get this data. We’ve literally brought back the patient a little while later and said, “Let’s just redo it and see for whatever reason we can get better data that day,” and we’ve got wonderful data that’s fit.
The analogy I would give folks, it’s kind of like many of our patients that have seizures have gone for EEGs and at some point in their life they say, “I have several normal EEGs or inconclusive, if you will, and then I finally got the one that showed my doc, yes, I have epilepsy. This is an abnormal EEG.” Can that happen to us? Yes, it can. But the nice thing is, especially if the person can do it without sedation or anything, is it’s an easy test to repeat.
Are you able to see the dendrites from the machine to determine damage to these after prolonged seizures?
We don’t visualize the actual structure, which is what they’re asking. We’re looking at function, if you will. We can get an idea if function has been changed in some other ways that I didn’t talk about today. There’s other ways we can use the MEG technology to look at function if it’s been altered. In the example I would give folks, again, if we look at analogies is I could give my car detail, take a picture of it, make it look great and show it to you, and then say, “Do you want to buy it?” You’d probably say, “Well, wait a minute, can I drive it first? Can I see if the air conditioning works?”
But if some of those functions weren’t quite so hot, that might change your thinking, right? They’re looking for, is there a change in structure? Whereas often what we really want to know is, is the function different in the patient, right? I mean, structure, yes, but we want to know how things are functioning.
Are there patients that cannot have MEG?
They’re rare in the modern era. The biggest ones I would say, and they’re pretty rare because the technology has shifted for a lot of our implants, I would say if a patient has had, gosh, probably like a really horrible head trauma where they had to have some kind of large bone flap that was metal plate because their head trauma was so bad and they had seizures from that. Even in the modern era, a lot of the ways that surgeons are doing that are compatible because they’ve gotten away from some of the older fashion kind of metal ones, because even with MRIs that’s a problem. They’ve kind of had to adapt for more current imaging where that’s less of an issue for us as well.
There are rare folks, to be candid. Even some of our patients that have cognitive issues that make it hard for them to understand the testing, if we can do sedation, unless they’re just behaviorally and cognitively so challenging that literally the parents tell us, the caregivers, it’s hard to even get them in a car to get to a hospital. Short of that, we can do it. There really are pretty rare exceptions in the modern world. I mean, we call patients, we kind of say, “Here’s what’s going to happen. Tell us about you,” most of those, if there’s any odd one there, we can tease it out before a patient’s driven to get a MEG or gone through the process, if you will.
Can you use prior MRI to superimpose the MEG or do you have to have sort of coincident testing done?
Prior MRI, I will say, sometimes can be used. Political answer here. The reason I say sometimes is it depends how it was done. To get the degree of resolution I showed you, we need what are called really thin cuts of the MRI to be done. Sometimes if they’re just doing what I would call a regular run-in-the-mill MRI, say you have headaches and got MRI, the cuts are much thicker. They don’t give us the details that we need to put our data on top of the structural picture.
That’s when we end up just saying we can just do part of the MRI over. We just need to do our structural part. We don’t need to do the whole 45-minute to hour MRI. It may just take us 10 minutes to do our part, for example. But if they’ve had a good structural MRI and we look at it, yeah, we can use that. Even my own patients, if they’ve had one six months, a year ago, as long as it wasn’t so long ago that we say, “Okay, things may have changed,” we can use those.
The information contained herein is provided for general information only and does not offer medical advice or recommendations. Individuals should not rely on this information as a substitute for consultations with qualified healthcare professionals who are familiar with individual medical conditions and needs. CURE Epilepsy strongly recommends that care and treatment decisions related to epilepsy and any other medical condition be made in consultation with a patient’s physician or other qualified healthcare professionals who are familiar with the individual’s specific health situation.