Options for Epilepsy Surgery
For some people with uncontrolled seizures, epilepsy surgery is an effective and important option to consider. This webinar will help patients and caregivers approach this difficult and sometimes confusing conversation with their doctors.
Advancements in surgery for treating epilepsy
Webinar presenter Dr. Kate Davis explores recent advances in epilepsy surgery, which have increased not only the types of surgeries available to patients but expanded who is an appropriate candidate for surgery. Dr. Davis also discusses the different tests performed as part of an epilepsy surgical evaluation and review current surgical options including resective surgery, laser ablation, and implantable devices.
Dr. Kate Davis is the Medical Director of the Epilepsy Surgical Program and Epilepsy Monitoring Unit at the University of Pennsylvania.
Q&A Transcript
How do you make sure that someone won’t have any new problems with memory or function after surgery?
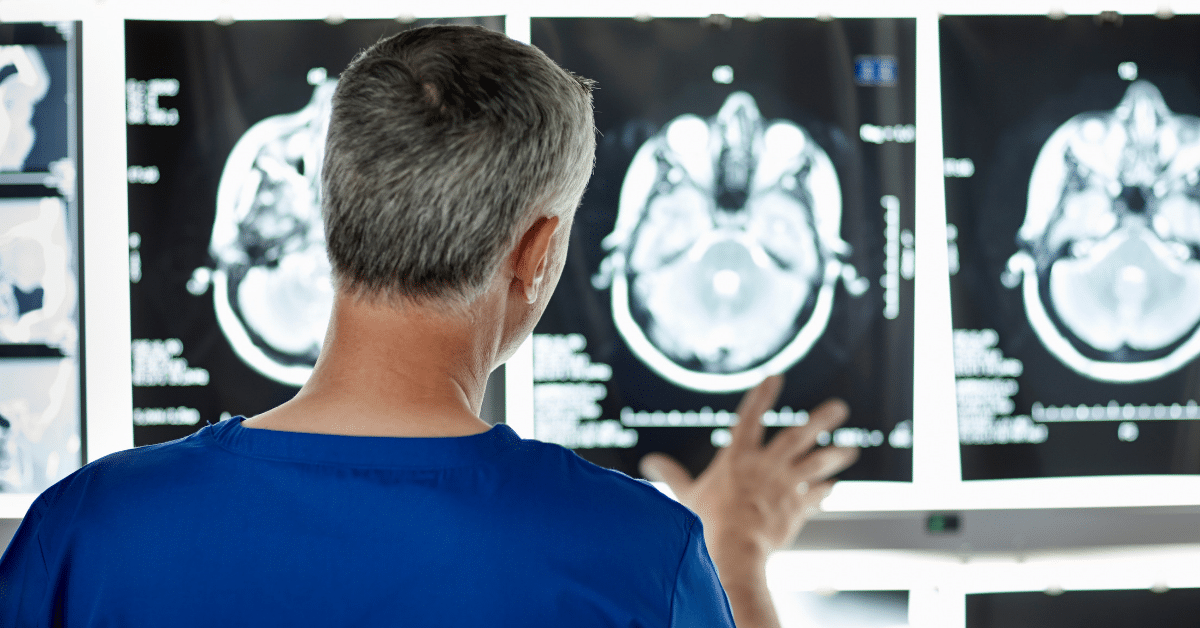
There are some parts of the brain that we don’t worry about it that much. However, there are a lot of parts that are really critical real estate. The neuropsychological testing is really helpful for us to determine whether there’s risk. There are also clinical factors that come into play. The age that the seizures started is really important. If seizure started really early in life, most people will have had a lot of reorganization of the brain and the areas of the seizures are usually not functioning. We can do some testing for that.
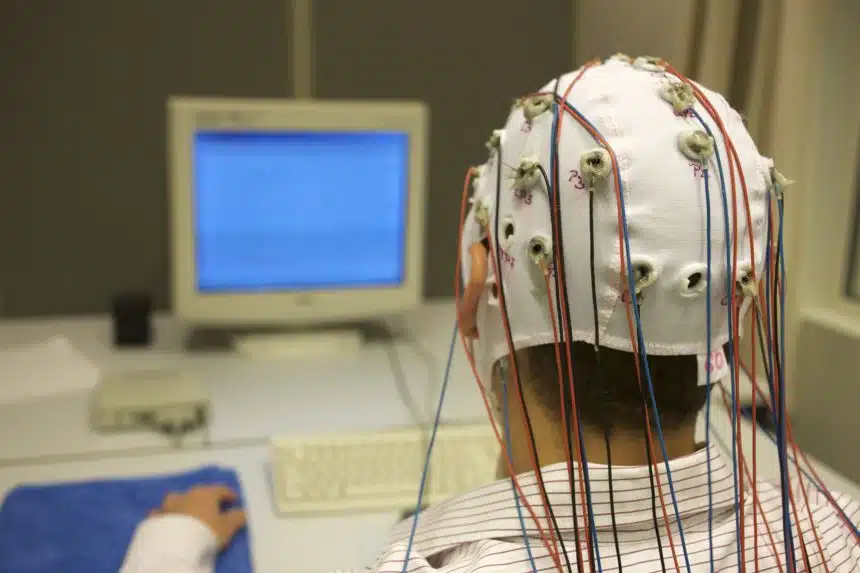
The functional MRI can look at where language is. We can also look at where motor function is, or what allows you to move your hands or your legs. With patients who have intracranial EEG, we can use those electrodes to map function. We do a combination of these things, plus our knowledge of what brain regions do in most people’s brains, and that can help us make an assessment of risk. Then that should be discussed by your treatment team with the family and the patient, if there is risk.
Are the ketogenic diet and AEDs are tried before surgery even becomes an option?
I briefly mentioned that the ketogenic (keto) diet is mostly used in pediatrics. I’m not a pediatric epilepsy specialist, but many pediatric patients will try the keto diet with seizure medications before considering surgery. Not all. That’s something definitely should be discussed with your treatment team. In adults, there’s very little evidence that the keto diet and other dietary therapy substantially helps with seizure. We do not have a trial of a diet therapy before we consider surgery because the data is really not there to support that decision.
Can deep brain stimulator (DBS) or RNS ever be implanted in pediatric patients?
I don’t know the specific age cutoffs because I don’t treat pediatrics, but the NeuroPace device is designed for the skull or the head of a seven-year-old or older. I think they are trying to change labeling to push the age back to pediatrics, and there are some centers that are implanting NeuroPace devices in pediatric patients. It is being done. Some of it is off label use, meaning it’s not under the FDA-approved label. The deep brain stimulator device is much newer, and I honestly don’t know if there are pediatric sites that are implanting that yet. I’m sure that we’ll learn that soon. I know that the pediatric epileptologists are very passionate about bringing these kind of technologies to their patients when they think it’s indicated.
Can you ever skip any of the tests, or is there a certain order that you always have to go through?
In the presentation, I went through a whole laundry list of tests. Not every patient needs each one of those tests. There is some variation in what centers use which tests. Some centers may not have availability of some tests, or have more experience with certain ones.
One test that I did not cover is a Wada test, which is done less frequently, but still at many centers is done. We will sometimes do Wadas in some patients. We will frequently do a functional MRI before doing that. Wada, just as an offside, is a test that’s been done for a very long time in epilepsy that is more invasive than the functional MRI, and that’s really one of the reasons there’s a move away from that test. Because it involves an injection of a drug that puts one side of the brain to sleep for a few minutes, during which time the neuropsychologist can do testing to look at function. Then you do it for the other side of the brain. That can give us information trying to determine the risk of the memory or language problems after a surgery, going back to the first question. In isolated cases, we are still doing Wadas.
I hesitate to say there’s a certain group of tests that each patient really needs. At a minimum, a brain MRI and EEG data is really done I think at every center. Then there’s some variation.
The information contained herein is provided for general information only and does not offer medical advice or recommendations. Individuals should not rely on this information as a substitute for consultations with qualified healthcare professionals who are familiar with individual medical conditions and needs. CURE Epilepsy strongly recommends that care and treatment decisions related to epilepsy and any other medical condition be made in consultation with a patient’s physician or other qualified healthcare professionals who are familiar with the individual’s specific health situation.