Children’s Hospital of Philadelphia Researchers Chart Natural History of Patients with SCN8A-Related Disorders
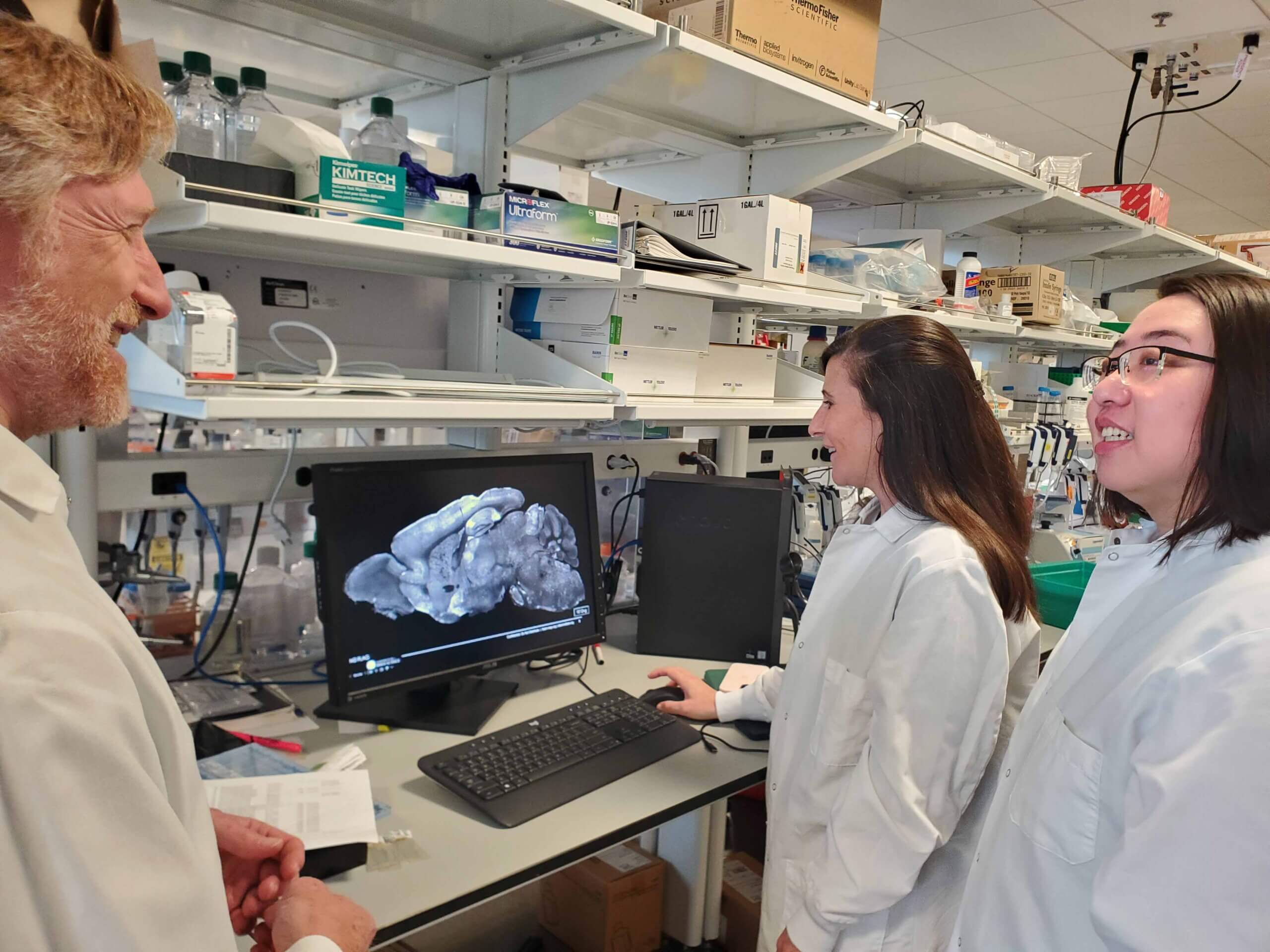
Featuring the work of Drs. Jillian McKee and Ingo Helbig, supported by in part by the CURE Epilepsy Rare Epilepsy Partnership Award for SCN8A, co-funded by The Cute Syndrome Foundation.
Researchers from the Epilepsy Neurogenetics Initiative (ENGIN) at Children’s Hospital of Philadelphia (CHOP) have completed a comprehensive natural history study of SCN8A-related disorders. The SCN8A gene encodes a specific sodium channel and variants in the gene have been linked to epilepsy syndromes and other disorders; notably, pathogenic variants in the SCN8A gene cause a spectrum of neurological conditions, including epilepsy, ranging in severity from mild to severe seizures, developmental delays, autism spectrum disorder and movement disorders.
Treatment of children with SCN8A mutations is challenging due to the lack of precision treatments and because the overall history of symptoms across the lifespan is poorly understood. In particular, the time course of clinical symptoms remains largely uncharacterized because of the wide range of variability and limited population sizes previously studied.
In this study, supported by a CURE Epilepsy Rare Epilepsy Partnership Award in partnership with The Cute Syndrome Foundation, researchers utilized electronic medical record data from 82 patients with SCN8A-related disorders and compared that information to a cohort of 2,833 patients with other genetic epilepsies.
The study found that patients with SCN8A-related disorders had more than 10-fold risk for developing bilateral tonic-clinic seizures as early as one year of age, a fact that was previously not appreciated. Gain-of-function SCN8A variants, which increase the activity of the sodium channel, lead to an increased risk of seizures as early as 6 months of age and global developmental delay as early as 3 months when compared to the broader cohort of SCN8A patients. Patients with loss-of-function variants, on the other hand, were more likely to have atypical absence seizures, which involve instances of “blanking out,” at around four years of age.
An understanding of these genotype-phenotype correlations will be critical when designing outcome measures and selecting participants for future clinical trials. Additionally, using sodium channel blockers to help manage SCN8A epilepsy was more effective in patients with gain-of-function variants as well as patients whose variants were not yet functionally characterized, suggesting that some of these variants may also be gain-of-function variants.
“Our analysis found that there is a significant developmental burden in SCN8A-related disorders with unique features that set these conditions apart from other epilepsies,” Jillian McKee, MD, PhD, an ENGIN epileptologist specializing in neurogenetic disorders at CHOP, said. “Knowing how unique features of SCN8A-related disorders develop over time is the first step towards readiness for clinical trials, so we can help our patients with these severe conditions.”