Understanding Epilepsy Main Menu
Table of Contents:
- What causes epilepsy?
- What are the symptoms of epilepsy?
- How do doctors identify the causes of epilepsy?
- When to see a doctor
- FAQs
What Causes Epilepsy?
Epilepsy is a complex condition that arises from abnormal electrical activity in the brain. It can manifest in various forms, from brief lapses in awareness to severe convulsions. While the exact cause of epilepsy in an individual may not always be clear, researchers have identified several common factors that can contribute to its onset.
On this page, you’ll learn about the six known causes of epilepsy and the diagnostic process physicians use to determine the underlying cause of a patient’s epilepsy.
What are the symptoms of epilepsy?
The symptoms of epilepsy can vary widely depending on the type of seizure and the areas of the brain affected. Common symptoms of epilepsy include:
Seizures
The hallmark symptom of epilepsy is seizures. Seizures can manifest in various forms, including:
- Generalized seizures: These seizures affect both sides of the brain and can cause loss of consciousness, convulsions, muscle stiffening, and rhythmic jerking movements.
- Focal seizures: Also known as partial seizures, these seizures affect only one part of the brain and can cause changes in emotions, sensations, or movements. Focal seizures may or may not lead to loss of consciousness.
- Absence seizures: Commonly seen in children, absence seizures cause brief lapses in awareness or staring spells. The person may appear to be staring blankly into space and may not respond to stimuli.
- Tonic-clonic seizures: Formerly known as grand mal seizures, these seizures involve loss of consciousness and muscle stiffening (tonic phase), followed by rhythmic jerking movements (clonic phase).
Learn more about seizure types
What Causes Seizures?
A seizure occurs when the brain experiences a sudden, uncontrollable surge of electrical activity, often triggered by factors such as epilepsy, head injuries, infections, high fever, or neurological disorders. This surge can lead to changes in behavior, movements, emotions, and levels of consciousness.
Why do seizures occur?
Seizures occur due to sudden, abnormal bursts of electrical activity in the brain, disrupting normal communication between nerve cells. They can be triggered by various factors, including epilepsy, head injuries, infections, high fever, stroke, brain tumors, genetic conditions, or imbalances in blood sugar or electrolytes. In some cases, the exact cause remains unknown.
Auras
Some individuals with epilepsy experience auras, which are warning signs that precede a seizure. Auras can manifest as visual disturbances, strange smells or tastes, feelings of déjà vu or jamais vu, or unusual sensations in the body.
Automatisms
During certain types of seizures, individuals may engage in automatic, repetitive behaviors known as automatisms. These behaviors can include lip-smacking, chewing, fidgeting, or repetitive movements of the hands or arms.
Loss of consciousness
Many types of seizures, particularly generalized seizures, can cause loss of consciousness. The person may appear confused, dazed, or unresponsive during and after the seizure.
Injuries
Seizures can sometimes lead to injuries, such as falls, cuts, or bruises, especially if the person loses consciousness or experiences convulsions during the seizure.
Postictal state
Following a seizure, some individuals may experience a postictal state characterized by confusion, fatigue, headache, muscle soreness, or memory loss. The duration and severity of the postictal state can vary depending on the individual and the type of seizure.
How do doctors identify the causes of Epilepsy?
In 2017, the International League Against Epilepsy (ILAE) introduced an updated tool for diagnosing epilepsy to help medical professionals worldwide provide the best possible care to their patients.
This system, called Classification of the Epilepsies, uses three levels to help physicians accurately diagnose an individual’s epilepsy: seizure type, epilepsy type, and epilepsy syndrome. As you can see from this graphic, it also emphasizes the importance of etiology, or causes, for each level, as this can determine which therapies are appropriate for a given patient.
International Framework for Classifying Epilepsies
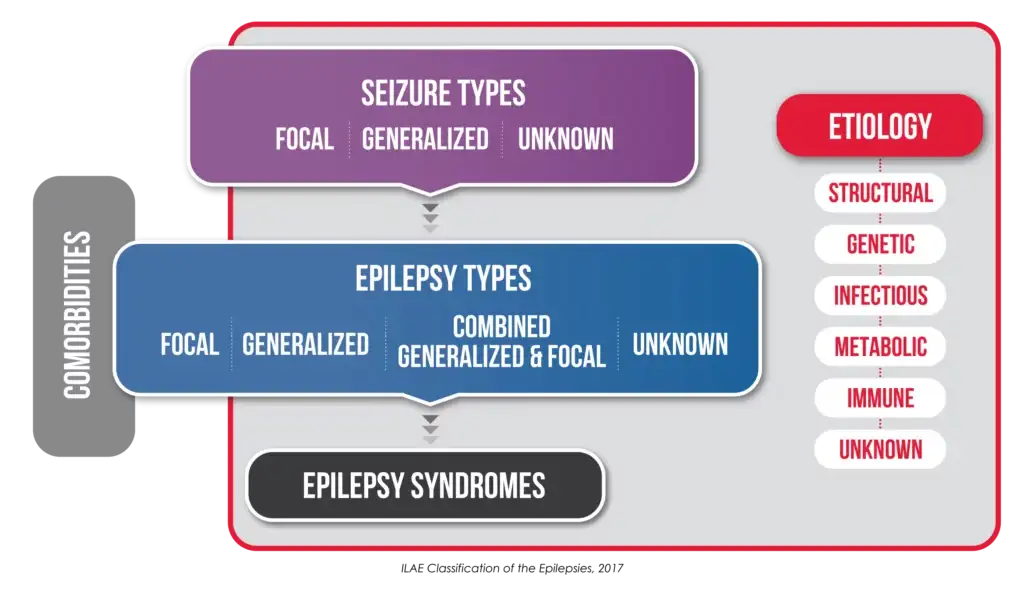
The causes of epilepsy are broken into six subgroups
- Structural
- Genetic
- Infections
- Metabolic
- Immune
- Unknown
Structural Etiology
A structural cause refers to brain abnormalities that are visible on structural neuroimages, such as an MRI. The underlying cause for this etiology can be acquired, genetic, or both.1 A person can acquire structural damage through stroke or head trauma, or it can be caused by genetic mutations during brain development.
Genetic Etiology
When a patient’s epilepsy is the direct result of a genetic mutation, they are considered to have a genetic etiology.1 Epilepsies with a genetic cause can be extremely diverse and the underlying genes are not always known. It’s important to note that genetic epilepsy does not automatically mean that it was inherited, or passed down from a parent, meaning that the mutations can be present in an individual, but not their parents.[2] According to the ILAE, there is a 50% chance that a patient with a de novo genetic mutation will pass this trait down to their children.
Infectious Etiology
When a patient has an infection in which seizures are a main symptom, they are considered to have an infectious etiology. Infections are the most prominent cause of epilepsy worldwide. An infection can cause epilepsy by directly impacting the brain cells of the person, or by releasing toxins that causes inflammation and seizures. Some examples of infections which can lead to epilepsy are: [1]
- Cerebral malaria
- Encephalitis
- HIV
- Meningitis
- Tuberculosis
- Zika virus
Metabolic Etiology
A metabolic disorder occurs when the process by which the body makes energy is disrupted or performs abnormally. Your body makes energy from the protein, carbohydrates, and fats in food that you eat. Chemicals break down the food into energy that can be used or stored. In some metabolic disorders, the abnormality affects the brain and increases the risk of epilepsy. Many metabolic epilepsies have a genetic origin (both inherited and de novo), though in extremely rare cases it can be acquired.
Identifying a metabolic cause can have significant implications on how epilepsy is treated.[1,3]
The ILAE has identified eight metabolic epilepsies that are important to know about:
- Biotinidase and holocarboxylase synthase deficiency
- Cerebral folate deficiency
- Creatine disorders
- Folinic acid responsive seizures
- Glucose transporter 1 (GLUT1) deficiency
- Mitochondrial disorders
- Peroxisomal Disorders
- Pyridoxine dependent epilepsy/PNPO deficiency
Immune Etiology
When your body recognizes a foreign agent (such as a virus), it protects itself by initiating an immune response. In some cases, your body may incorrectly identify itself as a foreign entity and begin attacking itself; if that autoimmune response causes you to have seizures, your epilepsy has an autoimmune etiology.5, 6 Examples of autoimmune epilepsy are Rasmussen’s encephalitis (also known as Rasmussen’s syndrome), limbic encephalitis, and GAD65 antibody-associated encephalitis.
Unknown Etiology
As the name implies, epilepsies with an unknown etiology have a cause that is not yet known. In other words, a person can be diagnosed with epilepsy, but the physician cannot make a specific diagnosis beyond that. In some cases, this is because there is still much we do not know about epilepsy; in other cases, this may occur because the patient does not have access to all of the proper diagnostic tests in order for their healthcare professionals to make an accurate diagnosis.[1]
When should you see a doctor about a seizure?
If any of the following happens during a seizure, it’s crucial to seek prompt medical attention:
- If the seizure lasts longer than five minutes.
- If breathing or consciousness does not return after the seizure ends.
- If another seizure occurs immediately after the first one.
- If there is a high fever.
- If the person experiencing the seizure is pregnant.
- If the individual has diabetes.
- If there are any injuries sustained during the seizure.
- If seizures persist despite taking prescribed anti-seizure medication.
Seeking medical help in these situations is important for proper evaluation and management of the condition.
Frequently Asked Questions (FAQs)
-
What causes seizures?
A seizure happens when a sudden, uncontrollable surge of electrical activity in the brain disrupts normal function. This can be caused by conditions such as epilepsy, head trauma, infections, high fever, or neurological disorders. As a result, a person may experience changes in behavior, movements, emotions, and levels of consciousness.
-
Can epilepsy be inherited?
Yes, certain types of epilepsy have a genetic component, and a family history of the condition can increase the risk.
-
Are all seizures caused by epilepsy?
No, seizures can have various causes, including fever, head injury, or medical conditions other than epilepsy.
-
Can epilepsy develop at any age?
While epilepsy can develop at any age, it is most commonly diagnosed in childhood or after the age of 65.
-
Is epilepsy a progressive condition?
In most cases, epilepsy is not a progressive condition, meaning it does not worsen over time. However, seizures may become more frequent or severe in some individuals.
-
Can epilepsy be cured?
While there is currently no cure for epilepsy, treatment options are available to help manage seizures and improve the quality of life for individuals with the condition.
Stay in touch
References:
- Scheffer IE, Berkovic S, Capovilla G, Connolly MB, French J, Guilhoto L, et al. ILAE classification of the epilepsies: Position paper of the ILAE Commission for Classification and Terminology Epilepsia. 2017 Apr;58:512-521.
- Steinlein OK. Genetics and epilepsy Dialogues Clin Neurosci. 2008;10:29-38.
- Pearson-Smith JN, Patel M. Metabolic Dysfunction and Oxidative Stress in Epilepsy International journal of molecular sciences. 2017;18:2365.
- Lin Lin Lee V, Kar Meng Choo B, Chung YS, U PK, Kumari Y, Shaikh MF. Treatment, Therapy and Management of Metabolic Epilepsy: A Systematic Review Int J Mol Sci. 2018 Mar 15;19.
- Geis C, Planagumà J, Carreño M, Graus F, Dalmau J. Autoimmune seizures and epilepsy J Clin Invest. 2019 Mar 1;129:926-940.
- Husari KS, Dubey D. Autoimmune Epilepsy Neurotherapeutics. 2019 Jul;16:685-702.
- Palace J, Lang B. Epilepsy: an autoimmune disease? Journal of Neurology, Neurosurgery &; Psychiatry. 2000;69:711.